Dermatology Center Becomes Fourth Clinical Elective Site in Canada
 St. George’s University has signed an agreement with North Bay Dermatology Centre to expand opportunities for fourth-year students to gain specialized clinical training in Canada. The center is SGU’s fourth clinical site in the country and one of the more than 70 clinical sites across North America.
St. George’s University has signed an agreement with North Bay Dermatology Centre to expand opportunities for fourth-year students to gain specialized clinical training in Canada. The center is SGU’s fourth clinical site in the country and one of the more than 70 clinical sites across North America.
Students who choose to do a rotation at North Bay Dermatology Centre, located in North Bay, Ontario, will gain general dermatology experience including treating patients with different types and stages of skin cancer as well inflammatory skin conditions. Run by Dr. Les Rosoph, the Centre also sees patients with psoriasis, dermatitis, rosacea, actinic keratosis, infections, connective tissue diseases, hair loss, acne, benign lesions as well as rare conditions.
“We are thrilled to add North Bay Dermatology to our growing list of impressive elective sites in Canada for students,” said Sandra Banner, SGU’s director of admissions for Canada, adding that she first met Dr. Rosoph in Grenada during Family Weekend when he was visiting his two daughters who are also med students at SGU.
“Through a two-to-four-week rotation with Dr. Rosoph and his team, aspiring physicians will be mentored in a highly specialized field and be able to do procedures once they are comfortable with the practice,” she said. “This is a wonderful opportunity for our students seeking to learn more about the dermatology discipline and further gain experience in the Canadian healthcare system.”
Dr. Rosoph said by accepting fourth-year students through the elective rotation, students can get a strong hands-on experience in the field of dermatology, which can be beneficial to those who choose primary care or a specialized field.
“I really believe in giving people opportunity and letting them make their own future,” Dr. Rosoph said. “For students that want to dive right in, we have lots for them to do.”
He also hopes to entice aspiring physicians to come north once they graduate.
“There’s really a need to bring doctors to northern Ontario,” Dr. Rosoph said. “Canada is so short of physicians once you leave the larger centers, and there are huge numbers of patients that never have access to primary care here. I’m hoping students will come and see Ontario and they will decide to relocate here.”
Located three hours north of Toronto, North Bay’s hospital and several clinics, including the dermatology clinic, serve as teaching units for the North Ontario School of Medicine’s undergraduate students and postgraduate programs. Dr. Rosoph also teaches at North Ontario School of Medicine.
SGU has been building its clinical network north of the US border. In November, St. George’s University finalized an agreement with Pembroke Regional Hospital in Ontario that offers fourth-year students a range of disciplines to choose from for their clinical electives. SGU also recently announced agreements in Ottawa with Ottawa Cardiovascular Centre and Booth Neurology Clinic—further expanding the opportunities available to students to broaden their skills and knowledge in preparation for residency. The first student to rotate at Booth Neurology Clinic began earlier this month.
Canadians have flourished at SGU and beyond: 18 Canadians who applied through the Canadian Resident Matching Service (CaRMS) secured residencies this year in competitive fields ranging from anesthesiology and emergency medicine to pathology and psychiatry.
Applications for placement at North Bay Dermatology beginning in January are now being accepted. The center has the ability to take two students at a time.
–Laurie Chartorynsky
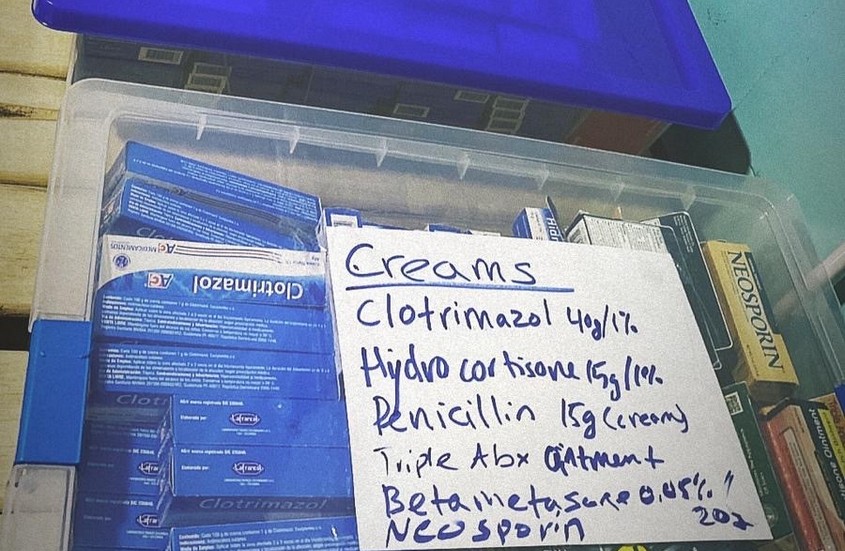
 The days were long yet the need to provide medical care to thousands of Venezuelan refugees living in Colombia was never more critical. Graduates from St. George’s University were among doctors and medical staff who recently travelled to Bogota and Cucuta to provide free medical services to the refugees.
The days were long yet the need to provide medical care to thousands of Venezuelan refugees living in Colombia was never more critical. Graduates from St. George’s University were among doctors and medical staff who recently travelled to Bogota and Cucuta to provide free medical services to the refugees.



 Raised in Houston, Texas, Katie Woodard, DVM ’14, grew up raising show pigs for
Raised in Houston, Texas, Katie Woodard, DVM ’14, grew up raising show pigs for 
 Adding to
Adding to 
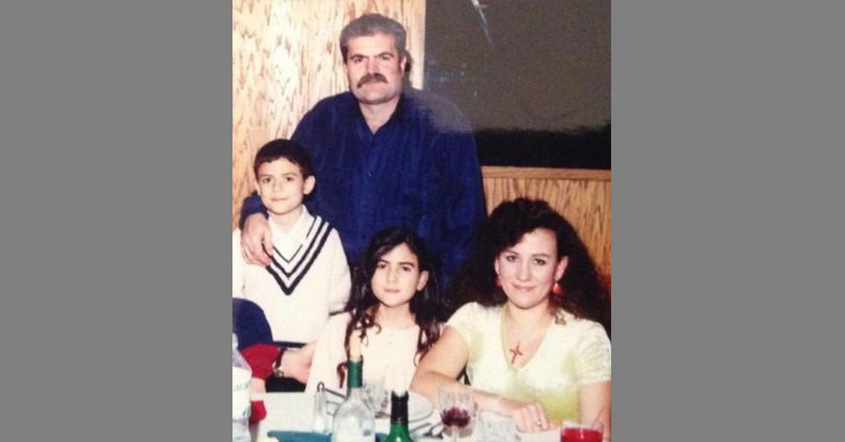
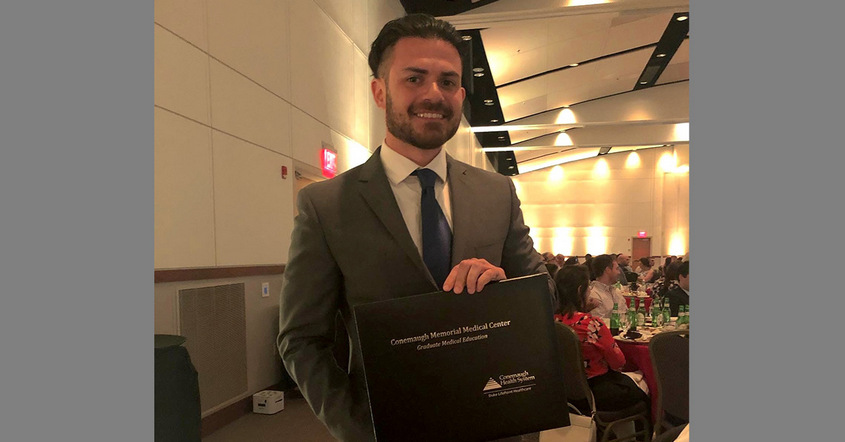
 A doctor delivered the news—cancer, an aggressive form. Joseph Di Como’s mother, a cornerstone of the family, would have to undergo surgery and many months of treatment.
A doctor delivered the news—cancer, an aggressive form. Joseph Di Como’s mother, a cornerstone of the family, would have to undergo surgery and many months of treatment.