St. George’s University School of Medicine graduate, Varshitha Tumkur Panduranga, MD ’24, couldn’t wait to start her internal medicine residency at SUNY Downstate Health Sciences University in Brooklyn, NY—her top choice for medical residency.
“During residency, I eagerly anticipate advancing my abilities as a physician, striving to refine both my theoretical understanding and practical skills,” Dr. Panduranga recently said. “Engaging in the intellectually stimulating realm of internal medicine, I aim to master deductive reasoning to deliver optimal care. The hospital where I have matched serves an underserved population and I am [also] eager to work in that environment and make a meaningful impact on their lives.”
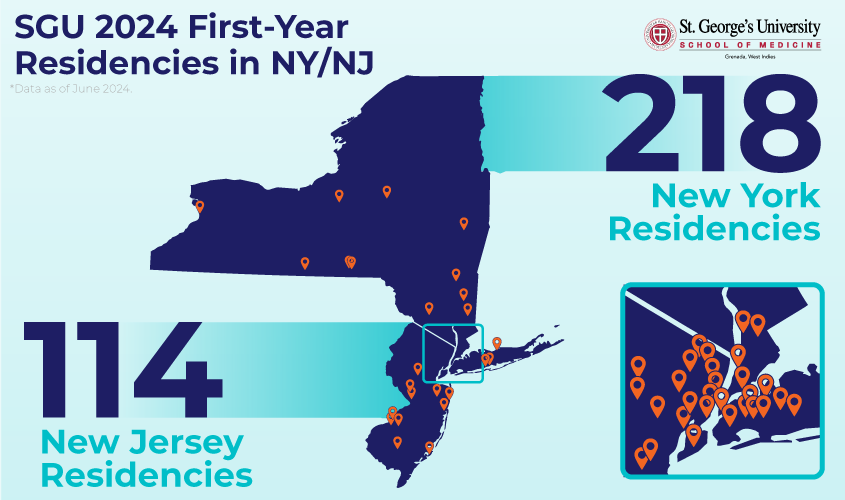
Dr. Panduranga is one of the 332 recent SGU graduates who began their postgraduate training at New York- or New Jersey-based hospitals this month. As residents, they will further train in specialties including: internal medicine, surgery, emergency medicine, family medicine, anesthesiology, ob/gyn, pediatrics, psychiatry, and more. She and her colleagues join nearly 10,000 SGU-trained doctors who have done postgraduate training in area hospitals over the years, according to SGU data as of June 2024.
Committed to communities
As the physician shortage in the US continues to be projected in the tens of thousands, SGU School of Medicine graduates are helping to meet the demand for doctors. For the 10th year in a row, SGU is the largest provider of new doctors to the US healthcare system and is helping address the physician shortage in the US.* Overall, more than 930 newly minted SGU MDs will embark on their intern year of residency training, offering a welcome addition at hospitals around the US.
The breadth of SGU’s impact on the healthcare workforce is none more evident than in New York and New Jersey. Many of the area’s hospital systems are located in communities where the need for doctors, particularly primary care physicians, is significant.
NYC Health + Hospitals, for instance, the largest municipal healthcare system in the country, serves over 1.2 million New Yorkers annually in over 70 locations, including 11 acute-care hospitals across the five boroughs. NYC Health + Hospitals serves some of the most marginalized populations in New York City, according to its 2022 Community Health Needs Assessment Report.
To help combat the physician shortage in the metro-New York area, the CityDoctors Scholarships Program, a partnership between SGU and NYC Health + Hospitals offers SGU med students full- or partial-tuition awards. It is designed to attract and educate students committed to serving in urban hospitals. To date, the CityDoctors program has made a career in medicine possible for more than 80 students, many of whom now practice in the communities in which they were raised.
In New Jersey, the need for primary care physicians is also critical, particularly for family physicians and general internists, according to a January 2024 report from the New Jersey Health Care Quality Institute. The report supports the notion of advanced primary care teams in New Jersey to ease the physician shortage.
Residents headed beyond the NYC metro areas, such as Barilee Abueh Idemudia, who is starting her internal medicine residency at the University of Buffalo, will also fill a vital need for physicians in New York and New Jersey.
“I am looking forward to making a meaningful impact on patient care, gaining hands-on experience, and honing my clinical skills while being a doctor my patient needs,” Dr. Idemudia said.
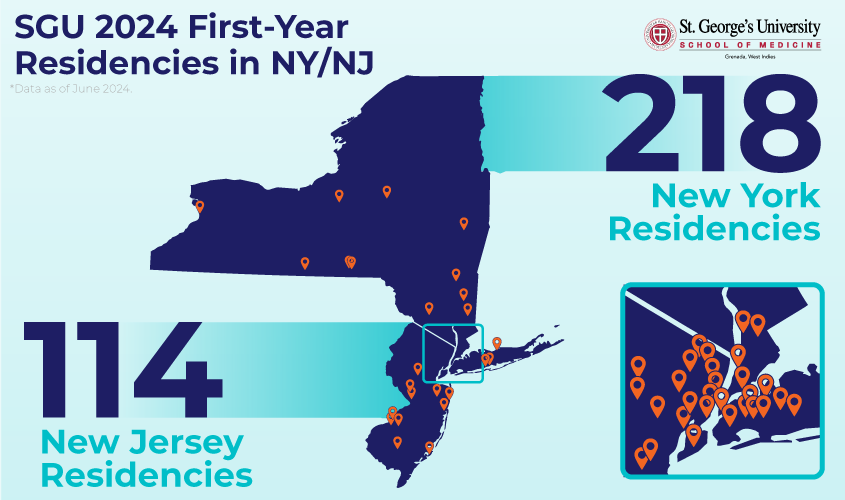
Over 300 SGU graduates began their residencies at New York- or New Jersey-based hospitals this month. They join nearly 10,000 SGU-trained doctors who have done postgraduate training in area hospitals over the years, according to SGU data as of June 2024.
Close to home
Many former SGU students also choose to continue their medical training in New York and New Jersey so that they can be closer to home.
“As we have a large number of students who hail from the New York-New Jersey area, many look to continue their education and training in areas where they grew up and have family,” said Dr. Robert Grant, SGU’s senior associate dean for clinical studies. “These newly matched students join a significant number of our alumni who are already practicing and contributing to patient care within the New York and New Jersey healthcare systems. We know they are well prepared and ready for the challenge of residency.”
Kelise Harris, MD ’24, began an anatomical/clinical pathology residency at Einstein/Montefiore Medical Center in Bronx, NY—not far from her hometown of Mount Vernon, NY.
Starting a residency close to home means Dr. Harris can better understand “what my patients needs are, the common pathologies they may present with, the circumstances that create these pathologies, and the pathways in which they may progress,” she said.
“It is a great feeling to be part of a healthcare system that is local to me and my community,” she added. “You form deeper, meaningful connections with your practice when it’s familiar territory; you no longer work from a place of trying to imagine yourself in someone’s shoes when you can draw from a well of genuine empathy because I am reminded that I am helping my neighbor.”
SGU in collaboration with three New Jersey hospitals—Jersey Shore University Medical Center, Hackensack University Medical Center, and St. Joseph’s Medical Center—offer an opportunity for incoming med students hailing from New Jersey to practice in their own communities. The SGU CARE Scholarship allows recipients to receive partial, half, or full tuition to attend SGU and then complete their clinical rotations at hospitals near their hometowns.
“I am looking forward to working and continuing to learn the specialty I love, in the community I grew up in, around doctors I shadowed and learned from as a pre-medical and medical student,” said Emily Rienzo, MD ’24, a first-year surgery resident at Jersey Shore University Medical Center and CARE scholarship recipient.
Developing professional relationships
With more than 75 clinical sites available for SGU students to train in the US, UK, and Canada, students have opportunities to develop professional relationships with the clinical faculty who work at these institutions, particularly in New York and New Jersey. These networking opportunities can potentially help lead to a residency position and even employment beyond residency, Dr. Grant added.
“Having completed most of my clinical rotations at St. Joseph’s Hospital, I am particularly excited about joining their team of phenomenal physicians,” said Justin Eadeh, MD ’24, a PGY-1 emergency medicine resident at St. Joseph’s University Medical Center in Paterson, NJ. “Their dedication to teaching and fostering a supportive learning environment is something I witnessed firsthand, and I am eager to further develop my skills under their mentorship. Additionally, the familial culture they uphold resonates deeply with me, and I am thrilled to become a part of such a close-knit community.”
Following residency training, SGU-trained doctors will become “a well-known and highly capable pool of physicians,” noted Dr. Grant. “They are the kind of doctors—predominantly primary care physicians—that these communities need.”
*As the medical school graduating the largest number of students per year, SGU places the largest number of graduates into residency programs each year, based on internal SGU graduate/expected graduate and residency placement data as of March 2024.
— Laurie Chartorynsky
Related Reading