Doctors Making a Difference: SGU Grads Travel to Colombia for Medical Mission Trip
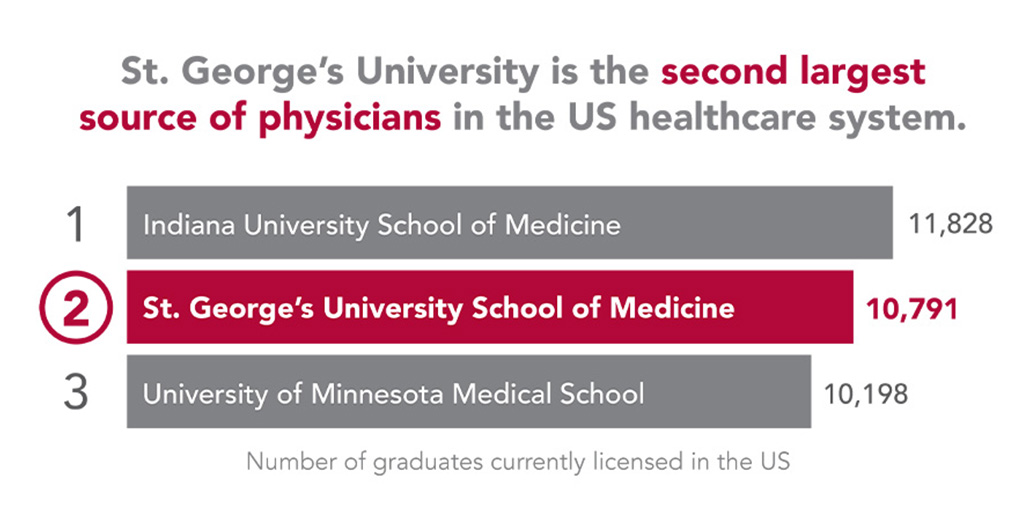
 The days were long yet the need to provide medical care to thousands of Venezuelan refugees living in Colombia was never more critical. Graduates from St. George’s University were among doctors and medical staff who recently travelled to Bogota and Cucuta to provide free medical services to the refugees.
The days were long yet the need to provide medical care to thousands of Venezuelan refugees living in Colombia was never more critical. Graduates from St. George’s University were among doctors and medical staff who recently travelled to Bogota and Cucuta to provide free medical services to the refugees.
Nathalie Briones, MD ’18, an emergency medicine resident at NewYork Presbyterian-Queens Hospital, was one of three SGU alumni who volunteered for the medical mission trip. “We saw a lot of communicable diseases, people dehydrated from having poor sanitation, parasites in children, and severe malnutrition,” said Dr. Briones. This was her second medical mission trip with trip organizers, Centurion Medical Missions. “We didn’t expect how acutely ill so many patients would be when we got there. Many of them were suffering from diseases that we had only ever seen before in our textbooks.”
Despite the dire conditions of the refugees in Colombia, she added that the team left each day more humbled and grateful than ever before. “The hardest part was hearing their stories about having to leave their homes. Many educated people—including doctors, lawyers, and engineers—were diminished to cleaning toilets or selling candy on the streets just to keep their children alive. These people once had everything, and now they have nothing. Many of us had to hold back tears during patient interviews because we knew that there was nothing we could do to change their circumstances.”
Added Dr. Briones: “Some moments you knew that you saved someone’s life by being there to treat them, and other moments you just wished you could do more.”
As one of the largest humanitarian crises in recent histories, more than four million Venezuelans—approximately 13 percent of the country’s population—have fled the country due to political instability, poor living conditions, and high crime since the revolution began in 1999. According to the UN Refugee Agency (UNHCR) and the International Organization for Migration (IOM), more than 1.3 million of those refugees have sought asylum in Colombia, leaving behind loved ones and most of their possessions to search for a better life.
However, once they arrive in Colombia, all is not what it seems. During a site visit this past spring, trip organizers visited one hotel where they encountered at least 100 refugees to a floor, with eight to nine people living in each room.
“All they have with them is what’s in their backpack,” said Gib Gerlach, vice president of humanitarian strategies for Centurion Medical Missions, a 501(c)3 nonprofit organization. “When they get to Colombia, their money is worthless. One of the greatest things they need is medical care and if they need it, they have no money to pay for it. We saw a great need to help out.”
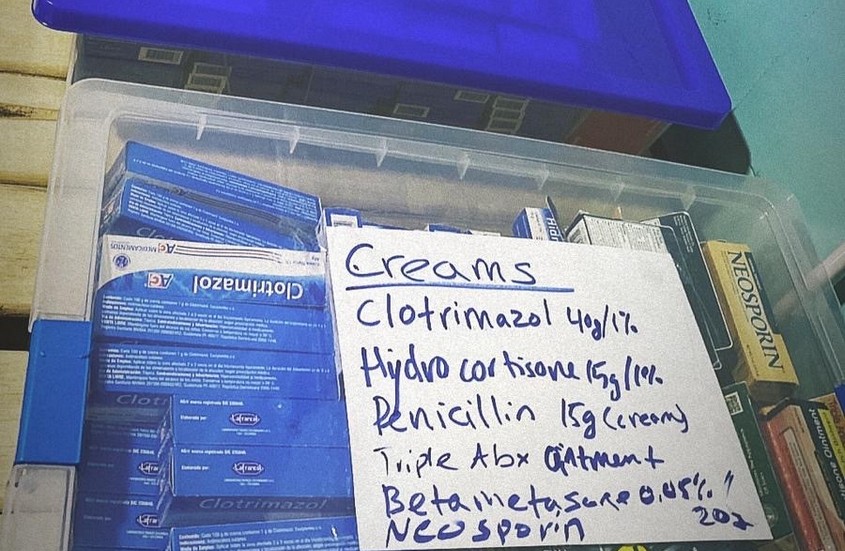
The trip, which took place December 9 to 13, included Dr. Briones, Chelsea Hoenes, MD ’13, and Yalda Hazrat, MD ’16, as well as a local physician, an emergency medical technician, and support staff. Volunteers flew in on Sunday, December 8 and spent the next four days seeing approximately 1,000 patients. The clinic welcomed all comers, including those with high blood pressure, acute respiratory issues, open wounds, malnutrition, urinary tract infections, and pregnant women, among other cases. The group purchases all of its medicine in country to help the local economy and to help build relationships, Mr. Gerlach said.
Dr. Hoenes also shared her perspective of the trip: “On arriving in the heart of Bogota, it is easy to see how the Venezuelan people are suffering one of the largest humanitarian crises in the world. Starvation and disease are their everyday reality. The medical care we provide is excellent but imperfect: the goal of our mission is to provide acute care, immediate access to imperative health resources, and hope, until permanent health infrastructure can be achieved for the growing refugee population.”
Centurion Medical Missions has previously performed medical clinics in La Vega, Dominican Republic. Of the six trips that Centurion Medical Missions has completed to La Vega since March 2018, 18 SGU doctors have so far travelled with the group, and many of them return for multiple trips. However, the need is so great in Colombia that the organization will be solely focusing on the country in 2020.
“We’re really happy to have to that relationship with SGU,” said Bill Honeycutt, founder of JET ICU, an air ambulance provider offering medical evacuation, medical repatriation, and other air medical transport services for patients worldwide and the parent company of Centurion Medical Missions. “It opens a lot of doors for the students and residents to build something down the road and eventually when they go into practice, they can continue to work to help thousands of people around the world.”
Dr. Briones said she hopes to inspire others to volunteer their services and training on future medical mission trips.
“I have always believed that every person in healthcare should try to do some kind of humanitarian work with underserved communities,” Dr. Briones said. “You really won’t know how much you can help until you go and see how much you actually do help.”
Visit SGU’s Instagram page for more images detailing the medical mission trip.
– Laurie Chartorynsky




 Raised in Houston, Texas, Katie Woodard, DVM ’14, grew up raising show pigs for
Raised in Houston, Texas, Katie Woodard, DVM ’14, grew up raising show pigs for  Adding to
Adding to 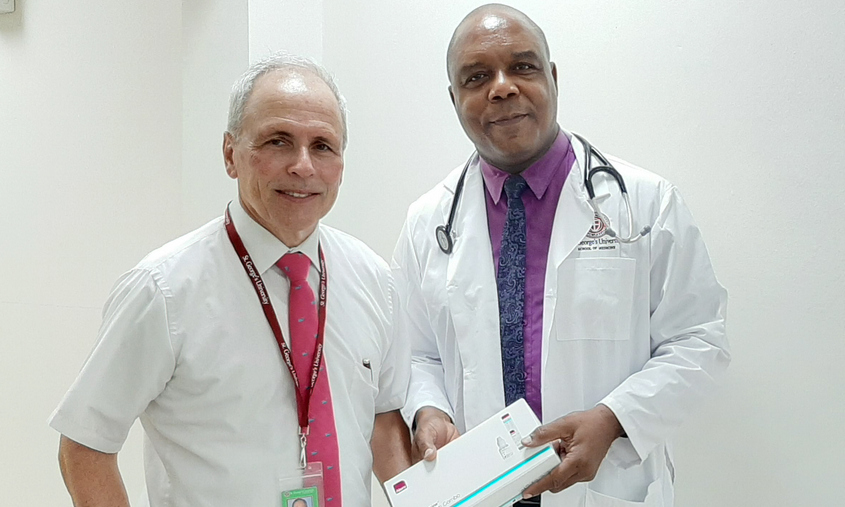 According to OB/GYN specialist Philip Lahrmann, MD ’81, if it wasn’t for St. George’s University, he wouldn’t be a doctor today. And as a proud graduate of SGU’s Charter Class, Dr. Lahrmann has dedicated more than 16 years to providing essential women’s health services to the place where he began his medical career almost four decades ago.
According to OB/GYN specialist Philip Lahrmann, MD ’81, if it wasn’t for St. George’s University, he wouldn’t be a doctor today. And as a proud graduate of SGU’s Charter Class, Dr. Lahrmann has dedicated more than 16 years to providing essential women’s health services to the place where he began his medical career almost four decades ago.
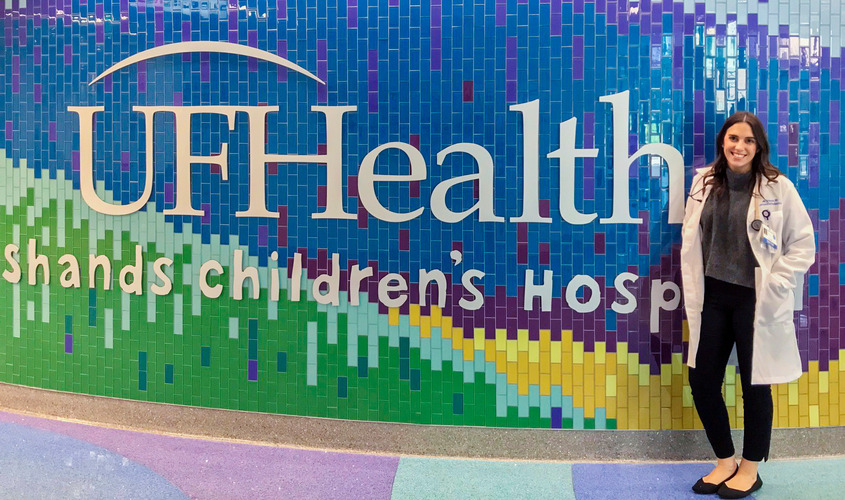 Madelin Brinson, MD ’19, was diagnosed with Type 1 diabetes when she was just 6 years old—following months of illness and unanswered questions of why she could not hold food down and was drinking gallons of water—literally—each night. The detection and ongoing management of her diabetes not only changed the course of her life forever, but strongly influenced her future career path, even at such a young age.
Madelin Brinson, MD ’19, was diagnosed with Type 1 diabetes when she was just 6 years old—following months of illness and unanswered questions of why she could not hold food down and was drinking gallons of water—literally—each night. The detection and ongoing management of her diabetes not only changed the course of her life forever, but strongly influenced her future career path, even at such a young age. A doctor delivered the news—cancer, an aggressive form. Joseph Di Como’s mother, a cornerstone of the family, would have to undergo surgery and many months of treatment.
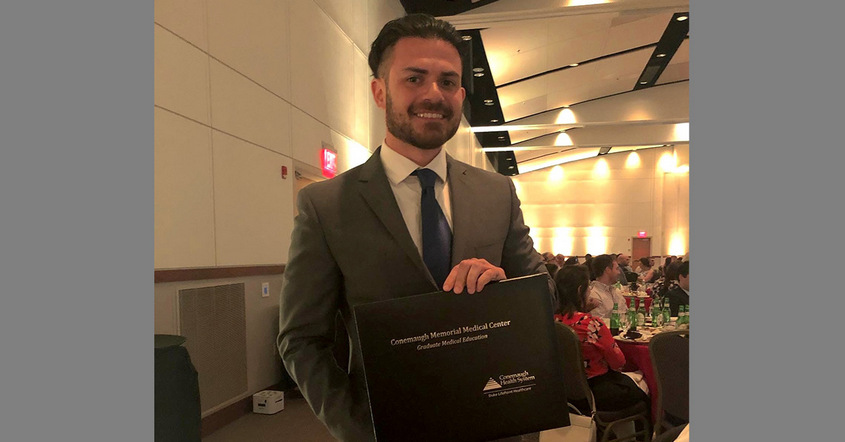
A doctor delivered the news—cancer, an aggressive form. Joseph Di Como’s mother, a cornerstone of the family, would have to undergo surgery and many months of treatment.